Linear IgA dermatosis (LAD), also known as linear IgA bullous dermatosis, is a rare autoimmune skin disorder that affects both children and adults. This disease causes the immune system to mistakenly attack the skin, resulting in blistering and rashes. Although it can be distressing, proper diagnosis and treatment usually help manage the condition effectively.
What Is Linear IgA Dermatosis?
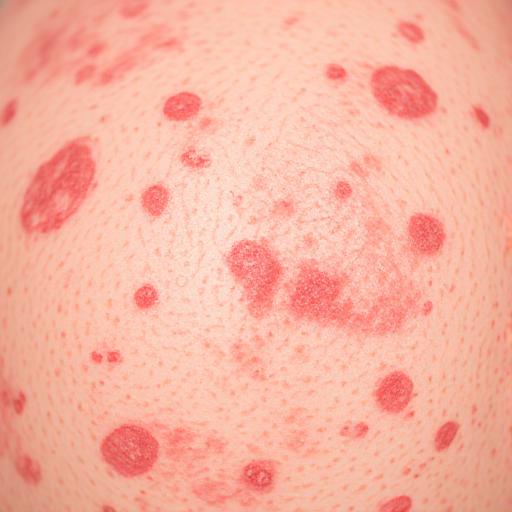
Linear IgA dermatosis is characterized by the formation of blisters and red, itchy patches on the skin. These symptoms happen because the body’s immune system produces antibodies called immunoglobulin A (IgA), which mistakenly target proteins in the skin. This causes separation of skin layers and leads to blister formation (Sardy et al., 2002).
There are two main types of LAD: one that affects children, often referred to as chronic bullous disease of childhood (CBDC), and one that occurs in adults. Though both forms look similar under the microscope and behave similarly, they tend to appear at different ages and may vary slightly in severity and location of blisters.
Causes and Triggers
The exact cause of LAD is not fully known, but it is considered an autoimmune disease. In this condition, the body’s immune system wrongly identifies parts of its own skin as harmful and attacks them. In LAD, the IgA antibodies line up in a linear pattern along a skin layer called the basement membrane zone, causing inflammation and blisters (Zone et al., 1998).
Certain medications can also trigger LAD, especially in adults. One of the most commonly associated drugs is vancomycin, an antibiotic used to treat bacterial infections (Kasperkiewicz et al., 2017). Other drugs like lithium, phenytoin, and captopril have also been linked to LAD in some patients. In such drug-induced cases, stopping the medication usually leads to improvement.
Symptoms and Diagnosis
The most noticeable symptom of LAD is the presence of fluid-filled blisters that can appear anywhere on the body. In children, these blisters often form around the mouth, genital area, and lower abdomen. In adults, they may occur on the trunk, arms, and legs. The blisters may group together and take on a pattern known as a “cluster of jewels” (Chanal et al., 2013). These can be itchy, painful, or even become infected if scratched or broken.
Diagnosis typically involves a skin biopsy, where a small sample of skin is removed and tested. Under the microscope, doctors can see a pattern of IgA antibodies along the skin layers. This test, known as direct immunofluorescence, is key to confirming LAD (Egan et al., 2001).
Treatment Options
Treatment for LAD focuses on stopping new blisters from forming and healing existing ones. The most commonly used medication is dapsone, an anti-inflammatory drug that works well in reducing the immune system’s attack on the skin (Wojnarowska et al., 2004). Dapsone is effective in most cases, but patients must be monitored for side effects, including problems with red blood cells and liver function.
If dapsone is not suitable or not effective, other medications such as corticosteroids (e.g., prednisone), sulfonamides, or immunosuppressants like azathioprine may be used. In drug-induced cases, simply stopping the triggering medication can lead to rapid improvement.
Living with LAD
Although LAD can be a chronic condition, many people experience periods of remission, especially children. With appropriate treatment, most patients lead a normal life. It is important to follow up with a dermatologist regularly, especially during flare-ups or medication changes.
In children, LAD often resolves by puberty. In adults, the condition may last longer but can be controlled with medication. Emotional support and patient education are also vital, as living with a chronic skin condition can impact mental health and self-esteem.
Conclusion
Linear IgA dermatosis is a rare but manageable skin disorder that results from the body’s immune system mistakenly attacking the skin. Though it can cause uncomfortable and unsightly blisters, with the right diagnosis and treatment plan, people with LAD can lead healthy lives. Ongoing research continues to uncover more about this disease, and advances in treatment are helping patients find relief with fewer side effects.
References
- Chanal, J., Ingen-Housz-Oro, S., Ortonne, N., Duong, T. A., & Bagot, M. (2013). Linear IgA bullous dermatosis: comparison between the drug-induced and spontaneous forms. British Journal of Dermatology, 169(5), 1041–1048. https://doi.org/10.1111/bjd.12404
- Egan, C. A., Zone, J. J., & Schroeter, A. L. (2001). Linear IgA bullous dermatosis: Clinical and immunopathologic findings in 49 patients. Journal of the American Academy of Dermatology, 45(4), 518–525. https://doi.org/10.1067/mjd.2001.114741
- Kasperkiewicz, M., Schmidt, E., Zillikens, D., & Hashimoto, T. (2017). Drug-induced linear IgA bullous dermatosis. Clinics in Dermatology, 35(4), 402–408. https://doi.org/10.1016/j.clindermatol.2017.03.012
- Sardy, M., Kostaki, D., Varga, R., & Simon, M. (2002). The target antigens in linear IgA bullous dermatosis. Journal of Dermatological Science, 28(3), 204–210. https://doi.org/10.1016/S0923-1811(02)00134-7
- Wojnarowska, F., Marsden, R. A., Bhogal, B., & Black, M. M. (2004). Chronic bullous disease of childhood and linear IgA disease of adults. In J. L. Bolognia (Ed.), Dermatology (pp. 489–495). Mosby.