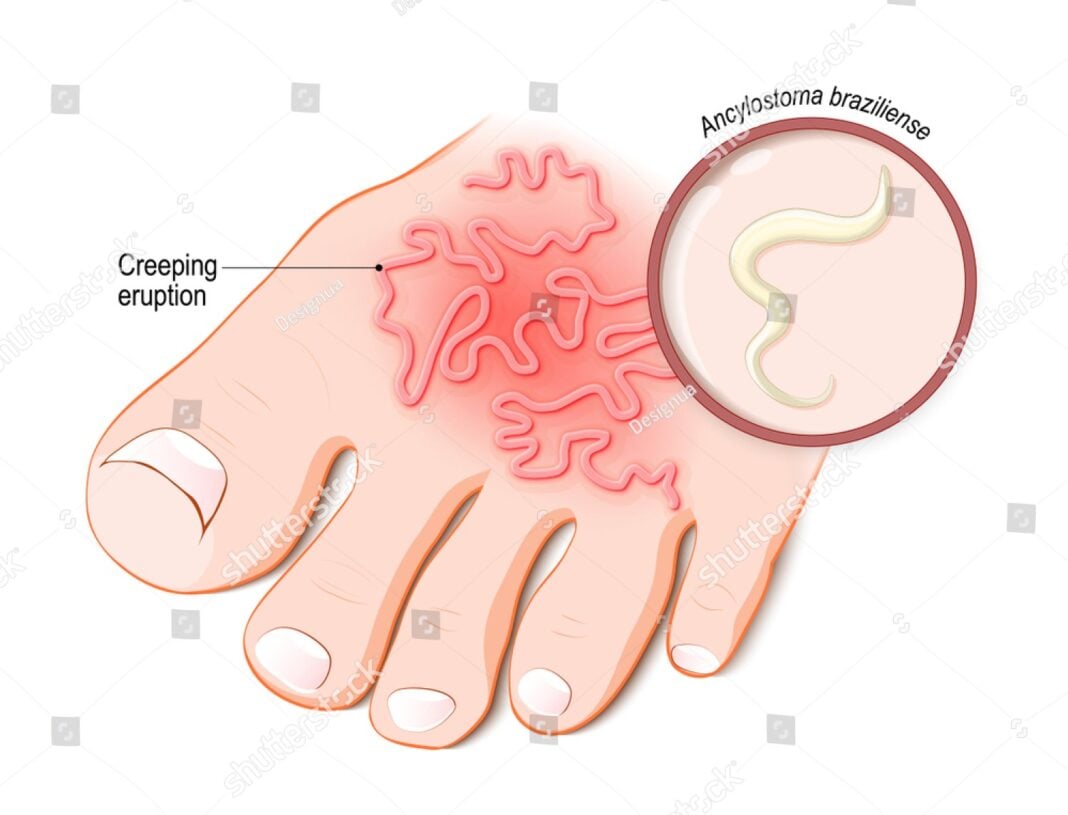
Cutaneous larva migrans (CLM) is a parasitic skin disease caused by the larvae of hookworms that normally infect animals, especially dogs and cats. It is often called “creeping eruption” because of the way the larvae travel under the skin, creating visible, winding tracks that can be itchy and uncomfortable. Although not usually life-threatening, CLM is a neglected condition that can cause a lot of distress, especially in people who live in or travel to tropical and subtropical regions (Blackwell et al., 2020).
Causes and Transmission
CLM is most commonly caused by the larvae of the animal hookworms Ancylostoma braziliense and Ancylostoma caninum (Centers for Disease Control and Prevention [CDC], 2022). These hookworms live in the intestines of infected dogs and cats, and their eggs are released into the environment through animal feces. In warm, moist soil, the eggs hatch into larvae. When humans walk barefoot or sit on contaminated soil or sand often in beaches or gardens the larvae can penetrate their skin, even through very tiny breaks or hair follicles.
Since humans are not the natural hosts for these larvae, they cannot complete their life cycle inside the human body. Instead, they wander aimlessly under the skin, causing the typical snake-like or winding rash (Heukelbach et al., 2018).
Symptoms and Appearance
The most obvious sign of CLM is the characteristic red, twisting rash that moves slowly over time, usually a few millimeters to a few centimeters per day. This rash is caused by the larva tunneling under the skin. It is often extremely itchy, and scratching can lead to secondary infections.
The rash usually appears on parts of the body that come into contact with contaminated ground especially the feet, buttocks, thighs, and hands. Some people may also experience mild swelling, pain, or a burning sensation at the site (Elder et al., 2021).
Who Is at Risk?
People who walk barefoot in sandy or moist environments, such as beaches, are most at risk. Travelers to tropical areas, especially those in South America, Southeast Asia, and the Caribbean, often get CLM during vacation and only notice the rash days or weeks later when they return home. Children, gardeners, and construction workers in endemic areas are also at higher risk (Blackwell et al., 2020).
Diagnosis
Doctors can usually diagnose CLM by looking at the rash and asking about recent travel history or exposure to potentially contaminated soil. Laboratory tests are rarely needed, although in complicated or unusual cases, a skin biopsy or dermoscopy might be performed to rule out other causes (Heukelbach et al., 2018).
Treatment
CLM often clears up on its own in a few weeks to months as the larvae eventually die. However, treatment is recommended to relieve symptoms and reduce the risk of infection from scratching. The antiparasitic medications albendazole or ivermectin are commonly used and are very effective (CDC, 2022). In some cases, a topical medicine like thiabendazole can be applied directly to the rash.
Antihistamines or corticosteroid creams may be used to control itching and inflammation. Keeping the area clean is also important to prevent bacterial infection.
Prevention
Preventing CLM involves avoiding contact with contaminated soil or sand. This can be done by:
- Wearing shoes or sandals when walking outdoors, especially in tropical areas.
- Using beach mats or towels when sitting or lying on sand.
- Keeping pets dewormed and discouraging them from defecating in public places.
- Promoting proper sanitation and cleaning up after pets.
Travelers should be particularly careful when visiting areas where animal control and sanitation may be poor (Elder et al., 2021).
Although CLM is rarely dangerous, it can cause significant discomfort and anxiety. With greater awareness, early diagnosis, and effective treatment, most people recover quickly. Public health efforts to control animal hookworms, improve sanitation, and educate travelers can help reduce the burden of this often overlooked tropical skin infection.
References
- Blackwell, V., Diaz, J. H., & Dario, R. (2020). Common skin diseases of travelers returning from tropical areas. Journal of Travel Medicine, 27(2), taz091. https://doi.org/10.1093/jtm/taz091
- Centers for Disease Control and Prevention. (2022). Cutaneous larva migrans (CLM). https://www.cdc.gov/parasites/zoonotichookworm
- Elder, D. E., Elenitsas, R., Johnson, B. L., & Murphy, G. F. (2021). Lever’s histopathology of the skin (12th ed.). Wolters Kluwer.
- Heukelbach, J., Feldmeier, H., & Hatz, C. (2018). Tropical dermatology: The neglected diseases. Clinical Dermatology, 36(2), 141–147. https://doi.org/10.1016/j.clindermatol.2017.11.001