Photosensitivity dermatitis, also known as photodermatitis, is a skin condition that occurs when a person develops an abnormal reaction to sunlight or artificial ultraviolet (UV) rays. While sunlight is essential for vitamin D production and general well-being, for some people, exposure to the sun can lead to itchy, red, inflamed skin. This condition is not just a simple sunburn it involves a deeper reaction between the skin and certain chemicals or medications.
What Is Photosensitivity Dermatitis?
Photosensitivity dermatitis is a type of skin inflammation triggered by exposure to UV light. This reaction happens because the skin becomes more sensitive to light due to external or internal factors. The result is an immune system response, leading to symptoms like redness, itching, swelling, or even blistering of the skin.
There are two main types of photosensitivity reactions: phototoxic and photoallergic.
- Phototoxic reactions occur when a chemical on the skin or in the body absorbs UV light and damages skin cells. This type is more common and usually happens soon after sun exposure.
- Photoallergic reactions, on the other hand, are less common and involve the immune system. They can appear a day or two after exposure and resemble eczema (Fotiou et al., 2021).
Causes and Risk Factors
Many different things can cause or increase the risk of photosensitivity dermatitis. These include:
- Medications: Certain antibiotics (like tetracyclines), anti-inflammatory drugs (such as ibuprofen), and even some heart medications can make the skin more sensitive to sunlight (Katta & Lim, 2016).
- Skincare products: Some sunscreens, fragrances, and cosmetics contain ingredients that trigger reactions when exposed to UV rays.
- Underlying health conditions: Autoimmune diseases like lupus can increase photosensitivity.
- Genetics: Some rare inherited conditions, such as xeroderma pigmentosum, make individuals extremely sensitive to sunlight.
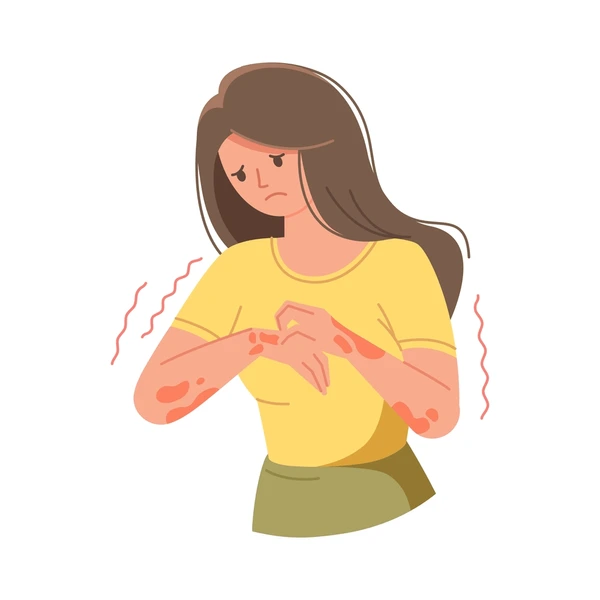
Symptoms of Photosensitivity Dermatitis
The symptoms can vary from mild to severe, depending on the person and the level of exposure. Common signs include:
- Redness and inflammation of the skin
- Itching or burning sensation
- Dry, scaly, or rough skin patches
- Blisters or hives in severe cases
- Skin darkening or discoloration after the rash heals
These symptoms usually appear on areas exposed to the sun as the face, neck, arms, and hands.
Diagnosis
Diagnosing photosensitivity dermatitis involves a detailed medical history and physical examination. Doctors may ask about recent sun exposure, medications, and skincare products used. Sometimes, specialized tests like photopatch testing or phototesting are done to find the specific trigger (Honari, 2019).
In photopatch testing, allergens are applied to the skin, and then the skin is exposed to UV light to see if a reaction occurs. This helps identify whether the reaction is photoallergic or phototoxic.
Treatment Options
The first step in managing photosensitivity dermatitis is to identify and avoid the triggers. Once the cause is found—whether it’s a medication or a skincare product—stopping its use can often improve symptoms.
Other treatment options include:
- Topical corticosteroids: These help reduce inflammation and itching.
- Antihistamines: These can relieve itching and reduce allergic reactions.
- Moisturizers: Keeping the skin hydrated helps in healing and reduces discomfort.
- Sun protection: Wearing protective clothing, wide-brimmed hats, and using broad-spectrum sunscreen (SPF 30 or higher) is essential (Katta & Lim, 2016).
In severe or chronic cases, dermatologists may prescribe medications that suppress the immune system.
Preventing Future Reactions
People with photosensitivity dermatitis must take extra steps to protect their skin:
- Avoid peak sunlight hours (10 a.m. to 4 p.m.).
- Use UV-protective clothing and sunglasses.
- Choose hypoallergenic skincare products and always test new products on a small patch of skin.
- Read medication labels carefully and talk to your doctor about sun-sensitivity risks.
Living with Photosensitivity Dermatitis
While this condition can be frustrating, many people manage it successfully with proper precautions and treatment. The key is awareness and prevention. Staying informed about what triggers your skin reaction and taking steps to protect yourself can greatly reduce flare-ups and improve your quality of life.
References
- Fotiou, C., Lazaridou, E., Vakirlis, E., Ioannides, D., & Rigopoulos, D. (2021). Photodermatoses: A comprehensive update. Clinical Dermatology, 39(2), 167–177. https://doi.org/10.1016/j.clindermatol.2020.11.005
- Honari, G. (2019). Photodermatitis: Diagnosis and management. Clinics in Dermatology, 37(5), 487–493. https://doi.org/10.1016/j.clindermatol.2019.04.004
- Katta, R., & Lim, H. W. (2016). Sunscreen photobiology: Molecular mechanisms and clinical implications. Journal of the American Academy of Dermatology, 75(3), 512–522. https://doi.org/10.1016/j.jaad.2016.01.055