If you’ve ever experienced eczema, you know it’s far more than just dry skin. It’s the relentless itch, the red, inflamed patches, and the emotional weight of feeling uncomfortable in your own skin. At the heart of this frustrating condition lies a key culprit: skin barrier dysfunction. Understanding what this means, and how it affects those living with eczema, is essential not just for treatment but for empathy and everyday care.
What Is the Skin Barrier?
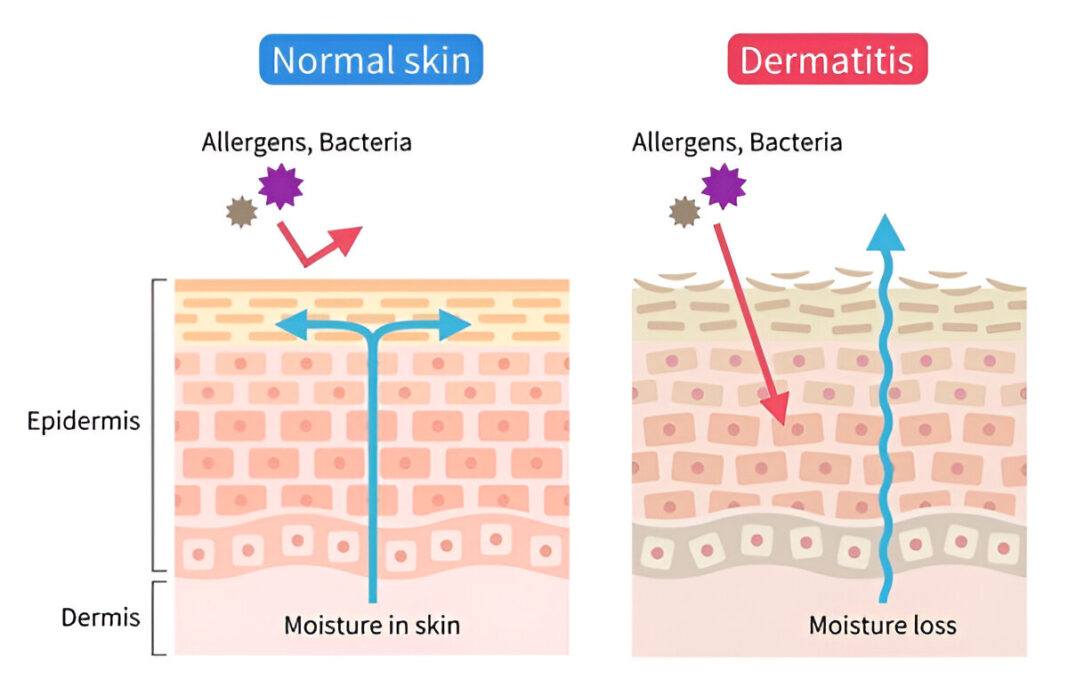
Think of your skin barrier as a brick wall. The skin cells (the bricks) are held together by lipids (the mortar), forming a protective layer. This barrier is crucial for keeping moisture in and harmful irritants, allergens, and microbes out (Elias & Steinhoff, 2008). When this wall is strong, your skin stays hydrated and resilient. But when it’s compromised, like in eczema, things go awry.
Eczema: More Than Skin Deep
Eczema, or atopic dermatitis, is a chronic inflammatory skin condition affecting up to 20% of children and 10% of adults worldwide (Nutten, 2015). While its exact cause is complex and multifactorial, one of the most consistent findings in research is that individuals with eczema have a weakened skin barrier.
When this barrier breaks down, skin becomes dry, vulnerable, and highly reactive. Everyday things like soap, sweat, wool fabrics, or even emotional stress can trigger intense flare-ups. The result? A vicious cycle of itching, scratching, and inflammation that’s physically and emotionally draining.
The Role of Filaggrin: A Missing Piece
One of the breakthrough discoveries in eczema research has been the role of a protein called filaggrin. This protein is essential for maintaining the skin barrier’s integrity. Mutations in the FLG gene, which produces filaggrin, are found in up to 50% of people with moderate to severe eczema (Palmer et al., 2006).
When filaggrin is deficient, the skin struggles to retain moisture and becomes more permeable to irritants and allergens. It’s like trying to keep a dam intact while pieces of the wall are missing. Eventually, things leak through.
Triggers and the Inflammatory Cascade
Once the barrier is compromised, allergens and microbes can easily enter, sparking an overactive immune response. This inflammation is what leads to the hallmark symptoms of eczema: redness, swelling, and that maddening itch. It’s not just the environment attacking the skin; it’s the skin reacting intensely due to its impaired defense system (Weidinger & Novak, 2016).
And while treatments like topical steroids or moisturizers help manage flare-ups, they don’t fully address the underlying barrier dysfunction, which is why eczema often recurs.
The Emotional Toll
It’s important to recognize that eczema doesn’t just affect the skin. It affects the whole person. For many, it means sleepless nights due to itching, social anxiety from visible lesions, and a constant, exhausting skincare routine. Parents of children with eczema often describe feeling helpless, watching their child suffer and trying every product on the shelf.
Understanding the science behind skin barrier dysfunction is not just an academic exercise. It’s a step toward compassion and better care.
Healing the Barrier: A New Focus
Fortunately, there’s growing recognition in dermatology that restoring the skin barrier is key to managing eczema effectively. Emollients rich in ceramides, free fatty acids, and cholesterol are now being recommended not just to soften the skin but to repair it (Cork et al., 2009).
There’s also excitement around barrier-targeted therapies that aim to strengthen the skin from within, such as topical agents that stimulate filaggrin production or enhance lipid synthesis.
Simple lifestyle changes can also support the barrier: using mild, fragrance-free cleansers, avoiding long hot showers, and applying moisturizers within minutes of bathing to “lock in” hydration.
A Hopeful Outlook
Though eczema can feel overwhelming, understanding the root cause of skin barrier dysfunction offers hope. It shifts the conversation from endlessly treating symptoms to proactively strengthening the skin’s natural defenses.
For individuals living with eczema, this knowledge empowers them to be kinder to their skin and to themselves. And for those supporting someone with eczema, it offers a deeper understanding of a condition that, although visible, runs deeper than the surface.
References
- Cork, M. J., Danby, S. G., Vasilopoulos, Y., Hadgraft, J., Lane, M. E., Moustafa, M., … & Ward, S. J. (2009). Epidermal barrier dysfunction in atopic dermatitis. Journal of Investigative Dermatology, 129(8), 1892–1908. https://doi.org/10.1038/jid.2009.133
- Elias, P. M., & Steinhoff, M. (2008). “Outside-to-inside” (and now back to “outside”) pathogenic mechanisms in atopic dermatitis. Journal of Investigative Dermatology, 128(5), 1067–1070. https://doi.org/10.1038/sj.jid.5701135
- Nutten, S. (2015). Atopic dermatitis: global epidemiology and risk factors. Annals of Nutrition and Metabolism, 66(Suppl. 1), 8–16. https://doi.org/10.1159/000370220
- Palmer, C. N., Irvine, A. D., Terron-Kwiatkowski, A., Zhao, Y., Liao, H., Lee, S. P., … & Smith, F. J. (2006). Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nature Genetics, 38(4), 441–446. https://doi.org/10.1038/ng1767
- Weidinger, S., & Novak, N. (2016). Atopic dermatitis. The Lancet, 387(10023), 1109–1122. https://doi.org/10.1016/S0140-6736(15)00149-X